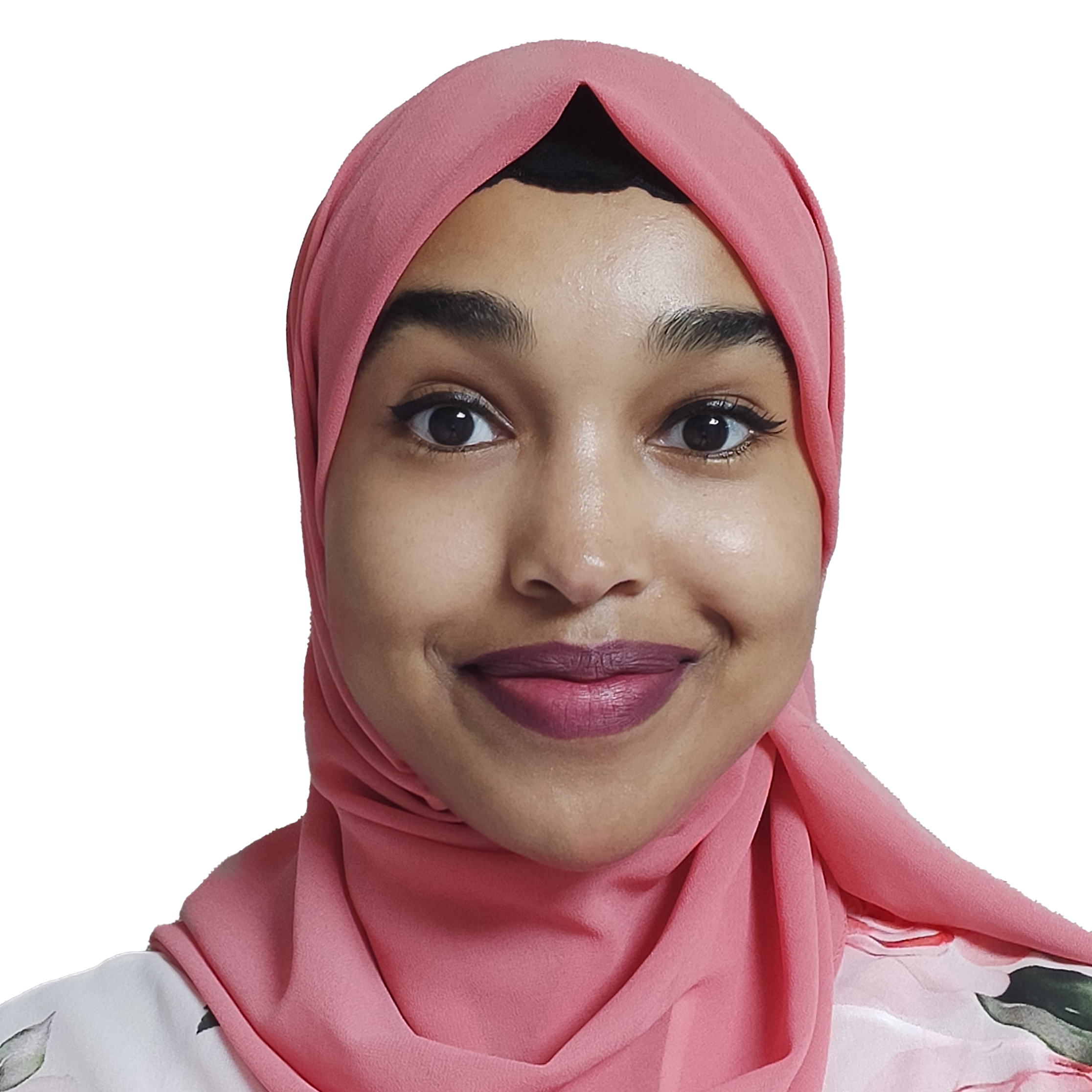
In our latest RCP next generation campaign blog, Dr Muha Hassan, RCP associate college tutor (ACT) and one of the winners of our 2025 ACT abstract competition shares how listening to resident doctor feedback led to a regional initiative to standardise clinic access – and why protected, hands-on learning time is essential for the future medical workforce.
Outpatient clinics are a vital part of medical training. They give doctors in training the chance to develop essential clinical and communication skills that will shape their future practice. However, survey feedback from resident doctors across the West Midlands highlighted significant variation in how NHS trusts organise clinic training opportunities.
‘Outpatient learning is vital, but for too many resident doctors, it means observing other people, rather than hands-on experience.’
Barriers to meaningful participation included limited room availability, inconsistent supervision and a lack of protected time. Some resident doctors described pre-scheduled clinic lists that left little space for active participation. Many described relying heavily on observation, with few opportunities to see patients themselves. While some trusts provided regular, protected clinic time, others relied on ad hoc arrangements, affecting the consistency of training. It became clear to us all that, despite the importance of outpatient learning, there was a need for a more structured and equitable approach.
Listening to resident doctor voices
As the local ACT and resident doctor representative on the internal medicine training (IMT) committee, I was well placed to hear these concerns firsthand. Resident doctor feedback was detailed and constructive – and I felt strongly that their voices needed to be acted on through a collaborative approach. I collected written feedback and shared it directly with college tutors (CTs) and training programme directors (TPDs), creating an opportunity for open discussion about how best to address the challenges.
‘Constructive feedback helped identify key barriers and set the agenda for change.’
We established a regional task and finish group of five CTs across the West Midlands and a resident doctor representative. Together, we developed a draft standard operating procedure (SOP) for IMT clinic training, designed to provide clear, region-wide guidance for resident doctors, trainers and trusts.
The SOP sets out curriculum expectations, defines supervision standards and outlines trust responsibilities for supporting clinic attendance. It also addresses barriers by recommending protected time, structured scheduling and flexibility for virtual clinics where appropriate. Stakeholder engagement has been central to this process, including discussions with TPDs, CTs and resident doctors. The SOP has now been formally submitted for regional review.
‘This project shows how ACTs can drive system-level improvements through collaboration.’
If adopted, the SOP has the potential to reduce variability, address barriers to clinic participation and improve the quality and equity of clinic-based training for IMTs across the West Midlands.
Lessons learned
Collaboration proved to be the key strength of this project. The feedback from resident doctors was clear and constructive, and the willingness of college tutors and TPDs to engage with the process gave the project real momentum. However, time constraints inevitably slowed progress, which means the SOP will not be implemented until next year.
Looking back, I would advise my past self to start consultation with resident doctors earlier and maintain more frequent communication throughout the process. System-level change takes persistence – and it requires building trust and buy-in from all stakeholders.
‘System-level change takes persistence – and early, frequent consultation makes a difference.’
Next steps
I will continue to support the implementation of the SOP, ensuring it delivers on its goal of equitable clinic opportunities for every IMT resident doctor in the region. My ambition is for all postgraduate training programmes to embed protected clinic time, with a small number of patients allocated for each resident doctor to see under supervision. This would create meaningful, hands-on learning experiences that move beyond observation and prepare resident doctors for independent practice.
‘Protected time is key to meaningful outpatient learning – and to the quality of care that future physicians will provide.’
Ultimately, ensuring protected outpatient opportunities is not just about meeting curriculum requirements. It is about recognising the impact that high-quality training has on workforce development and, most importantly, on patient care.