i. History
- Was the fall from height (eg over the rails of a raised bed) or because of syncope?
- Does the patient have a history of spinal fracture, or do they have/are at risk of osteoporosis or other spinal pathology?
- Have you already identified external evidence of head or facial injuries?
- Is the patient complaining of new neck pain?
ii. Examination
- Is there obvious new neck or spinal deformity?
- Palpate for midline tenderness.
- Any abnormal neurology?
- If C-spine injury is suspected at this stage using flowchart below (Fig 2) to assist decision, progress to immobilising C-spine and do not move neck further.
- Follow flowchart below (Fig 2) – if deemed safe, assess neck movement by asking patient to rotate neck 45° to the right and left.
iii. Management
Follow flowchart below (Fig 2) to determine whether a CT scan of the C-spine is required. Clear communication with radiology is required to organise appropriate manual handling for an immobilised patient.
Follow guidance for imaging as per NICE guideline NG232:
Fig 2. Algorithm for selecting people 16 and over for imaging of the cervical spine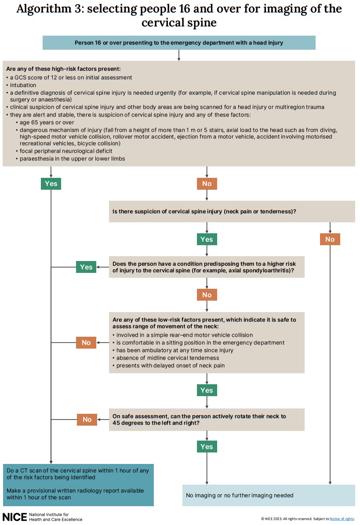
Figure 2. Algorithm for selecting people 16 and over for imaging of the cervical spine
- Click ‘Back’ on your browser to return to the Secondary survey section of the explanatory notes.





