i. History
Did they hit their head or was their fall unwitnessed? If so:
- Any visible injury?
- Any loss of consciousness?
- Are they on anticoagulants/ antiplatelets (excluding aspirin monotherapy), any clotting disorder?
- Any previous brain surgery?
- Any new reduction in GCS, loss of consciousness or seizures since fall?
- Is the patient complaining of new headache, memory loss, dizziness, double vision or vomiting after the fall?
- Any evidence of drug (including prescribed medication) or alcohol intoxication?
- Any evidence of irritability or altered behaviour?
ii. Examination
This involves a visual inspection and neurological examination:
- Look for scalp/ head laceration, contusions, evidence of fractures
- Eyes: visual acuity, pupil size and symmetry, haemorrhage of conjunctiva and/or fundi, ocular entrapment (eye movements)
- Any focal neurology?
- Clinical signs of a basal skull fracture: periorbital ecchymosis, retroauricular ecchymosis (Battle’s signs), rhinorrhoea or otorrhea (CSF leakage), and dysfunction of cranial nerves VII and VIII – facial paralysis and hearing loss - which may occur immediately or after a few days (6)
iii. For patients in community settings
If there is evidence of head injury or an unwitnessed fall, consider referral to the local emergency department if any of the following are present:
- Positive findings on history listed above (i. History)
- Any focal neurology
- Clinical concern
- Concern of patient/carer
- Inability to observe patient
If not using NHS transport, ensure that the patient is accompanied by a competent adult.
Shared decision making should be employed (8). An example of where this may be relevant includes patients with no other indication for imaging (of head, C-spine or any other injury) other than being on anticoagulation or antiplatelets (9).
iv. Investigation:
Follow guidance for imaging as per NICE guideline NG232:
Fig 1. Algorithm for selecting people 16 and over for a CT head scan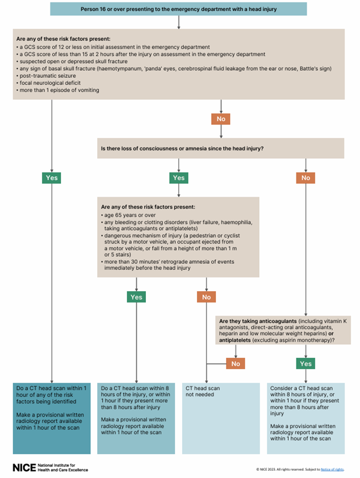
v. Management
In cases of a fall with head injury, or an unwitnessed fall, neurological observations should be documented every 30 minutes until a GCS of 15* is achieved. This should be followed by a frequency as for those patients with a GCS score of 15*: observations should be every 30 mins for 2 hours, every 1 hour for 4 hours, then every 2 hours for 24 hours.
This should include GCS score (separated into component parts – appendix 2), pupil size and reactivity, limb movements, respiratory rate, heart rate, temperature and blood oxygen saturation.
If any deterioration is observed, nursing staff should escalate immediately for reassessment, revert to half-hourly observations and follow the original frequency schedule as above.
Use of an appropriate head injury proforma / observation chart is recommended (10). The patient should be reviewed after 24 hours and a decision to continue or stop neurological observations should be made and documented.
Urgent reassessment and consideration of CT scan is required if there is:
- agitation or abnormal behaviour
- a sustained (for at least 30 minutes) drop of 1 point in GCS (give more weight to a drop of 1 point in the motor response of the GCS score)
- any drop of 3 or more points in the eye opening or verbal response scores of the GCS score, or 2 or more points in the motor response score
- severe or increasing headache, or persistent vomiting
- new or evolving neurological symptoms or signs, such as pupil inequality or asymmetry of limb or facial movement.
*If a patient is known to be disorientated at baseline due to a known cognitive impairment, GCS 14 can be considered their normal level and neurological observations followed as per GCS 15.
Anticoagulation including prophylactic heparin and antiplatelets should be reviewed. A senior decision maker should be involved if there is any doubt, and should undertake a risk–benefit analysis based on the individual patient. See notes on reversal of anticoagulation (section 6. Anticoagulation/antiplatelets) (11).
Refer to a neurosurgeon if there are any new and surgically significant abnormalities on imaging (refer to local referral pathway policy). Regardless of imaging, neurosurgical advice should be sought if any of the following is present:
- persisting coma (GCS 8 or less) after initial resuscitation
- unexplained confusion that persists for more than 4 hours
- deterioration in GCS after admission
- progressive focal neurological signs
- a seizure without full recovery; a definite or penetrating injury
- a cerebrospinal fluid leak. (10)
- Click ‘Back’ on your browser to return to the Secondary survey section of the explanatory notes.





